Atypical presentation of coronary disease in a young woman: imaging and lipidologyHarvey S. Hecht, T. J. Matarazzo, Manfred MoskovitzNew York, USAHECHT HS, MATARAZZO TJ, MOSKOWITZ M. Atypical presentation of coronary disease in a young woman: imaging and lipidology. Cardiol 2004;13(6):386–388 HECHT HS, MATARAZZO TJ, MOSKOWITZ M Atypický vzhľad ochorenia koronárnej artérie u mladých žien: zobrazovanie a lipidológia. Cardiol 2004;13(6):386–388
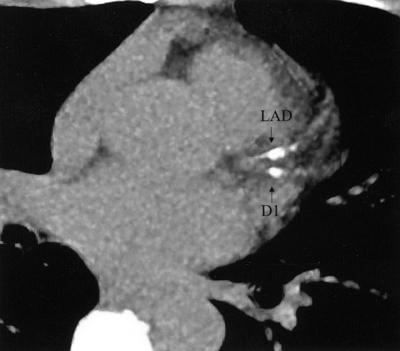
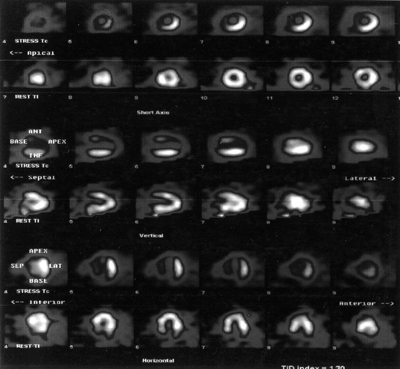
This case highlights many of the issues in contemporary preventive cardiology, particularly in women, with particular attention to imaging and lipidology. Clinical presentationThe patient is an anxious 41year old female with a low density lipoprotein (LDL) cholesterol of 150 mg/dl, a negative family history for premature coronary artery disease and no other risk factors. A stress echocardiogram was performed because of the high LDL cholesterol; it was normal. Two weeks later she developed intermittent back pain, not clearly related to effort. She was seen by several physicians, and her pain was attributed to anxiety, cervical disc disease or tendonitis. She was scheduled for orthopedic workup and an MRI of the neck and shoulder. On her own initiative, she sought cardiology evaluation. Her lipid profile, without pharmacologic therapy, was apparently excellent: total cholesterol 188 mg/dl, LDL cholesterol 112 mg/dl, high density lipoprotein cholesterol 50 mg/dl, triglycerides 132 mg/dl. The calculated Framingham 10 year risk was <1%. ImagingShe underwent Electron Beam Tomography (EBT) calcified plaque imaging (Figure 1): the calcium score was 95, in the left anterior descending (LAD), in the >99th % for her age, placing her in a high risk category. Based upon the EBT high risk classification, she underwent dual isotope nuclear stress testing (Figure 2) which revealed severe anteroseptal ischemia, followed by angiography and placement of a stent to treat a 95% ostial left anterior descending coronary artery stenosis (Figure 3), which did not appear thrombotic. She left hospital the next day. LipidologyAdvanced lipid testing (Berkeley HeartLab, Burlingame CA) revealed excessive small, dense LDL of 26% (normal <15%), high Lp(a) of 40 mg/dl (normal <20 mg/dl), and low HDL 2b of 15% (normal >30%). Homocysteine was 5.9 mmol/ml (normal <12 mmol/ml) and hs-CRP was 0.6 mg/L. 1. Atypical presentation of coronary artery disease in women: The back discomfort was an anginal equivalent. Atypical symptoms are more common in women, may not be taken seriously by physicians, and are often attributed to anxiety (1). 2. Limitations of stress testing: Stress testing is imperfect, particularly in women (1). Sensitivities range from ~67% for routine treadmill testing, ~80-90% for stress echocardiography, 85-90% for nuclear evaluation, and 90-95% for PET imaging. The absence of thrombus on angiography suggests that the critical stenosis was present at the time of the stress echocardiography, rather than the result of rupture or erosion of a plaque that was nonobstructive at the time of the stress test. The false negative result diverted attention from serious consideration of a cardiac etiology. 3. EBT is superior to Framingham risk estimates: The patient was in the very lowest Framingham risk category, and EBT correctly identified the extremely high risk. EBT has been consistently shown to be superior to Framingham Risk Score assessment (2). The latter is simply an estimate based upon risk factors; EBT is actual demonstration of atherosclerosis. The hs-CRP was normal, despite the symptoms and critical stenosis. Hs-CRP is a less powerful predictor of cardiac events than EBT demonstration of atherosclerosis (3). 4. Advanced lipid testing reveals unsuspected treatable disorders: The excess small, dense LDL, elevated Lp(a) and low HDL 2b are contributors to risk and should be treated with niacin. These disorders are only detectable through advanced lipid testing. Small dense LDL is the most common inherited lipid abnormality and is present in ~2/3 of patients with CAD and high risk primary prevention status. HDL 2b is the most cardioprotective component of HDL, and should comprise >30% of the total HDL in premenopausal women. Lp(a) is elevated in ~1/3 of high risk primary prevention and CAD patients (4). 5. Statins are mandatory in all high risk patients: The LDL cholesterol of 112 would not be considered atherogenic. Nontheless, statin therapy is mandatory because of the significant disease. Even if the plaque were nonobstructive, statins would be indicated because of the high risk EBT score, irrespective of the LDL, as demonstrated by the Heart Protection Study in high risk patients even with LDL cholesterol <100 mg/dl (5).
References1. Mosca L, Manson JE, Sutherland SE, et al. Cardiovascular disease in women. A statement for healthcare professionals from the American Heart Association. Circulation 1997;96:2468–2482.
|
|
|